 Revitalizing vision: Stem cell solutions unveiled
Revitalizing vision: Stem cell solutions unveiled
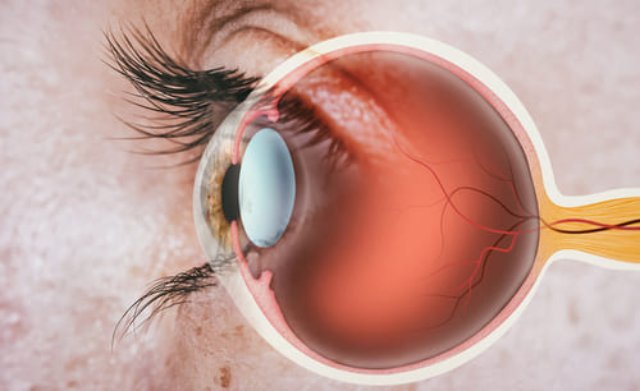
In the intricate landscape of ocular health, the Treatment of Optic Nerve Atrophy emerges as a critical focus. Recent advancements have paved the way for novel methodologies in addressing visual impairments, especially those stemming from retinal and optic nerve conditions. As we delve into this realm, it becomes essential to understand the underpinning technologies that are shaping the future of vision restoration.
Innovative Techniques in Cellular Restoration
Innovative techniques in cellular restoration have gained momentum, emphasizing the importance of understanding cellular microenvironments. The application of induced pluripotent stem cells (iPSCs) allows researchers to mimic the retinal architecture, thereby fostering the regeneration of damaged neural circuits. This regenerative approach not only enhances the potential for vision recovery but also invites a deeper examination of the cellular interactions involved.
Additionally, gene editing technologies, such as CRISPR-Cas9, present a paradigm shift by enabling precise modifications at the genomic level. This specificity is crucial in correcting inherited retinal disorders, offering a glimpse into tailored therapeutic strategies. The intersection of stem cell biology and advanced genetic techniques opens avenues previously deemed unattainable in ocular medicine, warranting further exploration and refinement.
The Role of Patient-Specific Biomaterials
The integration of patient-specific biomaterials holds significant promise in the realm of ocular regenerative therapies. Utilizing materials that are customized to the individual's unique biological profile enables a more conducive environment for stem cells to thrive. This personalized approach facilitates a delicate balance between biocompatibility and functionality, allowing the engineered scaffolds to mimic the native extracellular matrix, thus enhancing cellular integration and support.
Moreover, advanced 3D bioprinting techniques have emerged, allowing for the precise fabrication of complex structures that replicate the intricate anatomy of the eye. These innovations not only contribute to the restoration of vision but also provide a platform for studying cellular behavior in a controlled and relevant context. The ongoing refinement of these biomaterials will undoubtedly lead to more sophisticated and effective ocular therapies, albeit requiring continuous exploration of their long-term effects and interactions within the ocular environment.
Navigating Preoperative Protocols for Success
Preoperative protocols are critical in optimizing outcomes for ocular stem cell interventions. A comprehensive assessment of each patient's ocular history and physiological parameters establishes a personalized baseline. Essential components of this process often include:
- Utilization of high-resolution optical coherence tomography (OCT) for retinal layer analysis.
- Integration of dynamic visual field testing to gauge functional impairments.
- Evaluation of corneal thickness and morphology via scheimpflug imaging.
- Assessment of intraocular pressure variability through 24-hour monitoring.
These detailed evaluations enhance the understanding of the individual’s ocular condition, allowing clinicians to tailor surgical strategies more effectively. Moreover, optimizing systemic health factors, such as metabolic stability and immune system readiness, further contributes to procedural success, ensuring a robust foundation for subsequent regeneration efforts.
Long-Term Outcomes of Vision Regeneration
Long-term outcomes of vision regeneration through stem cell interventions present a complex tapestry of biological responses and anatomical integration. Research has underscored the persistence of regenerated photoreceptor cells, with findings suggesting that their survival rates can be influenced by the anatomical site of implantation and the microenvironment engineered around them. Studies have also noted the significance of neurotrophic factor availability, as it plays a pivotal role in sustaining cellular viability over extended durations.
Moreover, the ongoing evaluation of visual function restoration requires advanced imaging techniques and functional assessments that extend beyond traditional metrics. Factors such as synaptic plasticity and the establishment of new neural pathways are critical in mapping the trajectory of visual recovery. Understanding these longitudinal aspects elucidates the intricate dynamics governing stem cell therapies, highlighting the necessity for continuous adaptation in treatment protocols to optimize outcomes.
The intersection of advanced cellular methodologies, personalized biomaterials, and meticulous preoperative evaluations creates a nuanced approach to vision restoration. As the field progresses, the insights gained from long-term outcomes will undoubtedly inform future innovations, driving the evolution of regenerative therapies within ocular medicine.

